Talking about my drugs
I’ve had ankylosing spondylitis for more than 12 years. In all that time, why didn’t anyone tell me that I could take other analgesics on top of my anti-inflammatory medications?
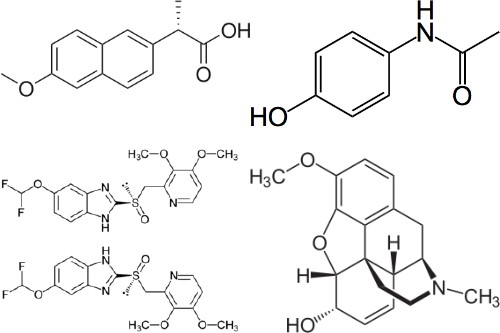
Some background. I first started showing the symptoms of AS in the spring of 1997, and was diagnosed at the end of the year. Before my diagnosis, I made do with ibuprofen; after my diagnosis, I went on high-dose naproxen, which made the symptoms — the pain, stiffness and inflammation — manageable most of the time. From mid-2000 to early 2001, feeling experimental, I tried a few other NSAIDs — celecoxib, indomethacin, diclofenac — as well as sulfasalazine, but they were less effective: celecoxib wasn’t nearly strong enough; indomethacin did funny things to my head; diclofenac did funny things to my liver. So I went back to naproxen, the side effects of which — heartburn and ringing in the ears — were tolerable. In 2003, my doctor added pantoprazole, a proton pump inhibitor that practically eliminated the heartburn (something the misoprostol I’d been taking prior to that never could do).
So things stood until last week. If the naproxen didn’t always vanquish the pain and inflammation, it worked well enough most of the time. Flares came, frequently in the spring and fall, and they were frequently awful, but I managed to manage. I kept telling myself that while the dosage is constant, the disease isn’t.
But this year (as I mentioned last month), it’s been particularly rough. I haven’t been able to tell whether the disease has been getting worse — I’ve had rough patches before — but whatever the arc, it hasn’t exactly been good.
I came to the conclusion that I was not managing my disease very well. And that thought frightened me. I’ve been clinging to naproxen as the least bad option. No other NSAID worked as well with as few side effects, but that wasn’t to say that it worked well enough, often enough. And I was not yet prepared to consider the TNF blockers, which are expensive, difficult to administer, and have their own side effects. (I imagine that I’ll be on one of them eventually, but the longer I can put off that day, the better.) And opiate-based painkillers scared me even more: I would take any amount of pain to avoid psychological side effects or an addiction to oxycodone or hydrocodone.
I mentioned this situation to my doctor last week, during my annual physical. The option we settled on was acetaminophen — plain, ordinary, over-the-counter stuff — with a prescription for co-codamol (i.e., acetaminophen plus codeine, also known as Tylenol 3) when it gets worse.
Me: “You mean I can take acetaminophen on top of naproxen? I didn’t know I could do that.”
(Apparently I can!)
I’d always been worried about drug interactions — obviously, too worried — but had never gotten around to asking whether I could take drug X with drug Y. It’s been a while since I had an annual physical during a flare, or this would have come up sooner. (I’d like to think so, anyway.)
So last Friday I took the first acetaminophen I’d had in more than a decade (excepting, of course, the amount found in cold medications like Neo-Citran — the stuff is in everything). Took one of the prescription pills with codeine before going to bed.
I slept for ten hours and woke up at eight the next morning — the longest bout of uninterrupted sleep I’d had in years. On Saturday a friend looked at me in amazement: the bags under my eyes were gone; I don’t think she’d ever seen me without them.
Let me back up and say something about sleep. AS improves with activity and worsens with rest, which means that it gets worse as you sleep and is at its worst in the morning. When I was on ibuprofen, I was lucky to get five hours’ sleep a night: I’d wake up in the middle of the night in abject pain, and would be unable to get back to sleep. With naproxen, that five-hour limit was extended to eight hours, most of the time. I could function, but I could never sleep in: if I tried sleeping past eight hours or so, I’d wake up in pain. (It’s one hell of an alarm clock, let me tell you.) That also meant that if I got short on sleep for some reason, it would take me forever to get caught up again. I spend a lot of time in sleep deficit, particularly when I’m working.
It may have just gotten a lot easier to stay caught up on my sleep.
Let me also say something about pain. The tendency of the medical profession is to focus on the disease’s symptoms, not necessarily to manage the pain. In the context of AS, that means controlling two things: joint fusion (my spine is essentially trying to fuse itself solid) and inflammation. Controlling the pain is, I guess, a pleasant side effect of combatting the disease. Now, fusion and inflammation aren’t necessarily connected. In my case, I have a good deal of inflammation to deal with, but it turns out that the fusion may not be progressing at all: my flexibility tests from last week are identical to similar tests taken five years ago. So my joints are in flare a lot, but they show no sign yet that they’re intending to fuse solid any time soon. From one perspective, that means I’m doing well — but I’m also hurting like hell, exhausted and missing work.
The acetaminophen-and-codeine combo will do nothing to address the symptoms of my disease, but they will help me take care of the basics: sleep and pain. Which, to be perfectly honest, I haven’t been looking after as well as I should. It’s still early going and I still have to fine-tune the pill-taking, but I’ve got some reason to be optimistic here, for the first time in years. And all because I got the go-ahead to take some fairly common and innocuous painkillers — not some $15,000-per-year exotic miracle drug. If they work, fantastic. If they don’t — well, we’ll try something else.